Quality patient care. Whether you’re part of an FQHC or private practice, everyone can agree it’s the No. 1 objective. How well your clinic delivers on that objective depends largely on the health of its revenue. Likewise, your clinic’s revenue is highly influenced by the quality of your patient care.
If you’re like many clinics today, you feel the pressure of a progressing economic downturn, heightened competition, and increased operating costs. On the patient side of the business, a tightening workforce is resulting in symptoms such as staff overwhelm, growing wait times, and patients that are falling through the cracks.
A March 2022 study by the American Nurses Foundation and the American Nurses Association found that 52% of nurses are considering leaving their current position due primarily to insufficient staffing, work negatively affecting their health and well-being, and an inability to deliver quality care.
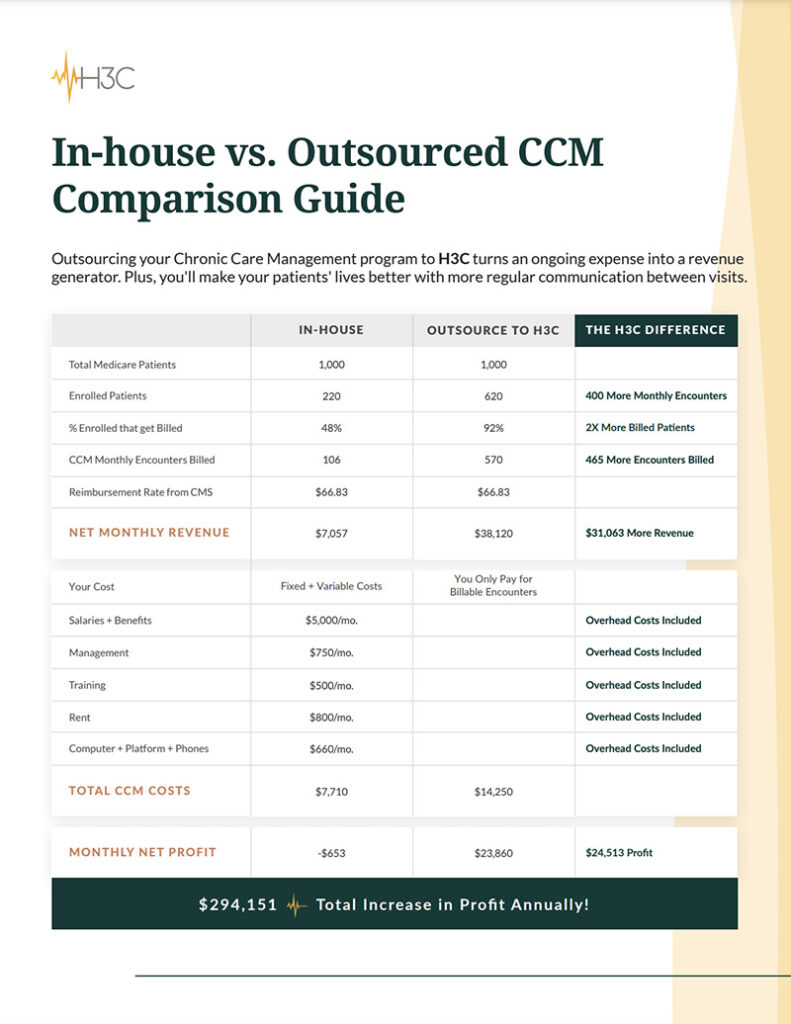
With a lot of suggestions circulating about how to increase clinic revenue and streamline staff workloads—namely significant investments in tech—only one opportunity stands out as an efficient solution for achieving both increased income and improved patient outcomes: a chronic care management program.
That sounds like more work for my already overworked staff.
It’s hard to imagine asking your staff to manage yet another new system or technology—even if it benefits your patients. The good news is that a chronic care management program doesn’t need to be difficult or burdensome to implement. Furthermore, it can integrate with your existing systems. When done correctly, a good CCM program should relieve the pressure on your nursing team and generate new revenue for your clinic.
Let’s take a step back and look more closely at the functionality of a CCM program.
What is a CCM program?
Chronic care management (CCM) provides preventative services to individuals on Medicare who have two or more chronic conditions. CCM offers your eligible patients a regular connection with their provider, helping them take a more proactive, empowered approach to their health and wellness.
A CCM program can aid your clinic in facilitating earlier interventions among patients, encouraging compliance with medication regimens, supporting lifestyle improvements, reinforcing scheduled appointments, and even reducing the number of hospitalizations, complications, and unnecessary ER visits that your patients may face.
How does a CCM program work?
Whether in-house or outsourced, a CCM program should be staffed by qualified, licensed clinicians who conduct monthly patient encounters. While the path to success varies by clinic, here are four common steps toward an established CCM program:
- Identify patients who qualify and make an initial connection to introduce the program.
- Enroll interested patients.
- Provide monthly phone calls for each enrollee from a dedicated team who understands the patient’s current medical challenges and can provide compassionate care, support, and encouragement.
- Integrate patient assessments from each call directly into your clinic’s EMR system, enabling more constructive conversations between providers and their patients during office visits.
How CCM services benefit patient outcomes?
Patients enrolled in a CCM program report stronger connections with their healthcare team. Not only will a CCM program improve patient engagement and compliance, but it also gives your team additional information in order to see the broader picture behind each patient’s current medical situation. Additionally, patients receiving CCM services are more likely to:
- Engage with their clinic and providers.
- Have a higher rate of medication compliance.
- Experience fewer hospitalizations.
- Feel safe, resulting in a closer relationship with their doctor and clinic.
The National Center for Biotechnology Information (NCBI) reports that patient-centered care has been correlated with reduced pain and discomfort, faster physical and emotional recovery, as well as improved outcomes and quality of life.
How CCM services benefit providers?
By facilitating regular touchpoints, CCM services foster a more trusted relationship between provider and patient. This enables your team to identify new developments in a patient’s health and pinpoint higher-risk patients. With increased patient engagement and fuller information, your staff is better equipped to pre-empt conditions that often result in acute care and emergency room visits.
On the business side, CCM services are eligible for Medicare reimbursements. This creates an additional revenue stream that can be used to further improve patient care at your clinic.
How to support your staff and achieve better outcomes?
Here’s a look at the ways some of our H3C partners have applied these funds to better support their staff and ultimately achieve better patient outcomes.
Hire More Staff
With 1,000 enrolled Medicare patients, an FQHC could see up to $920,000 in additional gross revenue this year. Based on average salary figures from ZipRecruiter, that additional revenue means you could add:
- 7 FQHC nurse practitioners, or
- 6 FQHC dentists, or
- 5 FQHC physicians, or
- 15 FQHC nursing staff members.
Boost Staff Morale
Nurses and clinic staff are overwhelmed, and 44% of nurses say that burnout is affecting their ability to care for their patients. By using revenue from a CCM program to invest in additional nurses, technology, and support staff, you can ease the burden on your existing team members—creating further savings in staff acquisition and retention.
Invest in Technology
According to this article from Hartman Advisors, FQHCs will continue to see increased demand as ongoing economic fluctuations cause many Americans to consider more affordable and accessible healthcare options. In order to keep up, clinics must implement effective technology to:
- Streamline their operations,
- Shift certain tasks away from staff through automation,
- Provide more accessible services, such as telehealth appointments, and
- Improve patient outcomes.
Facilitate Virtual Visits
Many chronic care patients put off routine check-ins because of the time commitment or physical toll required to attend an in-person appointment. A CCM program can keep patients engaged and solve simple issues, like medication refills and specialist referrals, over the phone. And, your clinic can serve more patients with less overhead.
Reduce Missed Appointments
We know that more engaged patients are more likely to follow care plans and take medications, which leads to better maintenance of or improvement in their chronic conditions. H3C contacts your patients at least once a month, every month, to keep them engaged with their care plan and remind them of any upcoming appointments. Your patients will keep more appointments, more often, or our staff will help them reschedule or solve challenges that are preventing them from attending.
Make Onsite Appointments More Meaningful
Our CCM staff sends all encounter information, including risk stratification reporting, directly to your EMR. Your care team has up-to-date, detailed information about a patient’s progress and symptoms entered every month. H3C’s risk stratification and reporting structure ensure that doctors and nurses have a full health history for the patient, allowing every appointment to make a greater impact on the patient’s health.
How H3C Can Help
Current statistics show that 40% of adults have more than one chronic disease. An effective way to help patients manage these conditions is by providing easy access to resources, positive reinforcement, and regular follow-ups.
When patients have access to continuous care through CCM services and regular appointments, plus access to testing and imaging services that the revenue from CCM can help you provide, illnesses are detected and treated at an earlier stage. This leads to a reduction in hospital stays and other adverse outcomes.
H3C provides outsourced CCM services that can help your clinic scale and start earning new revenue in as few as three weeks. Once your clinic has more revenue, especially revenue from a source that requires no additional capital investment, you can begin investing in new equipment and personnel to better serve your patient population.
For more information on CCM programs, see our complete guide.
Get in touch with H3C today to discuss the ways a CCM program could support your clinic’s revenue, staff satisfaction, and patient population.