Chronic care management (CCM) is a key component of successful patient care. A good CCM program can help your clinic scale to facilitate preventative care among more Medicare-qualified patients, which leads to fewer hospitalizations, complications, and unnecessary visits to the emergency room.
However, a challenge faced by many clinics is the difficulty of assigning appropriate billing codes for each service. Accurate and consistent coding is critical to your clinic’s revenue, but it’s also incredibly time-intensive for your staff. In this article, we’ll provide a comprehensive guide to chronic care management billing codes—including who qualifies, what qualifies, and when to bill—so you can make sure your practice is properly compensated.
CCM Code 99490
Who qualifies to use this code? Patients with two or more non-complex chronic conditions that are expected to last at least 12 months, or until the death of the patient.
What qualifies as a billable encounter? At least 20 cumulative minutes of care for non-face-to-face care per patient per calendar month—which does not necessarily mean per 30 days. Thus, if you bill for an encounter on Jan. 27, you can also bill for an encounter on Feb. 15. As another example, if you provide qualifying care on March 10 for 10 minutes and again on March 20 for 15 minutes, you can bill under this code after reaching the minimum 20 cumulative minutes of non-face-to-face care.
When can you bill for this code? CCM billing code 99490 reimburses time spent by clinic staff, under the direction of a physician or qualified healthcare professional, on basic patient coordination services that support patient accountability. This may include arranging follow-up appointments, refilling prescriptions, or requesting and updating medical records. All services must be included in the patient’s care plan.
CCM Code 99487
Who qualifies to use this code? Patients with two or more complex chronic conditions that are expected to last at least 12 months, or until the death of the patient. This type of patient requires moderate- to high-complexity medical decisions and thus more staff time.
What qualifies as a billable encounter? At least 60 cumulative minutes of care for non-face-to-face care per patient per calendar month.
When can you bill for this code? CCM billing code 99487 reimburses time spent by clinic staff, under the direction of a physician or qualified healthcare professional, on establishing, revising, or monitoring a patient’s comprehensive care plan.
CCM Code 99489
Must be paired with CCM Code 99487
Who qualifies to use this code? Patients with two or more complex chronic conditions that are expected to last at least 12 months, or until the death of the patient.
What qualifies as a billable encounter? Each additional 30 minutes of non-face-to-face care (per patient per month) that is provided over and above the 60 minutes provided under CCM Code 99487.
When can you bill for this code? CCM billing code 99489 cannot be listed on its own. It must meet the same conditions as CCM Code 99487 and should be reported when a patient requires an additional 30 minutes of care in a single calendar month after Code 99487 has been exceeded.
CCM Code G0511
The go-to CCM code for rural health centers (RHCs) and federally qualified health centers (FQHCs).
Who qualifies to use this code? Patients with two or more non-complex or complex chronic conditions that are expected to last at least 12 months, or until the death of the patient.
What qualifies as a billable encounter? At least 20 cumulative minutes of clinical staff time.
When can you bill for this code? In 2018, Code G0511 effectively replaced Code 99490 and Code 994987 for RHCs and FQHCs. This code reimburses time spent by clinic staff on basic chronic care management services as well as behavioral health integration services provided by a qualified health care professional.
Remember: One Bill Per Qualified Professional Per Month
It’s important to also remember that even though services can be provided by a variety of clinic staff, only one qualified healthcare professional can bill for CCM services per patient per calendar month. This can include a physician, clinical nurse specialist, nurse practitioner, or physician assistant. Additionally, non-physicians must be legally authorized and qualified to provide CCM in the state in which services are provided.
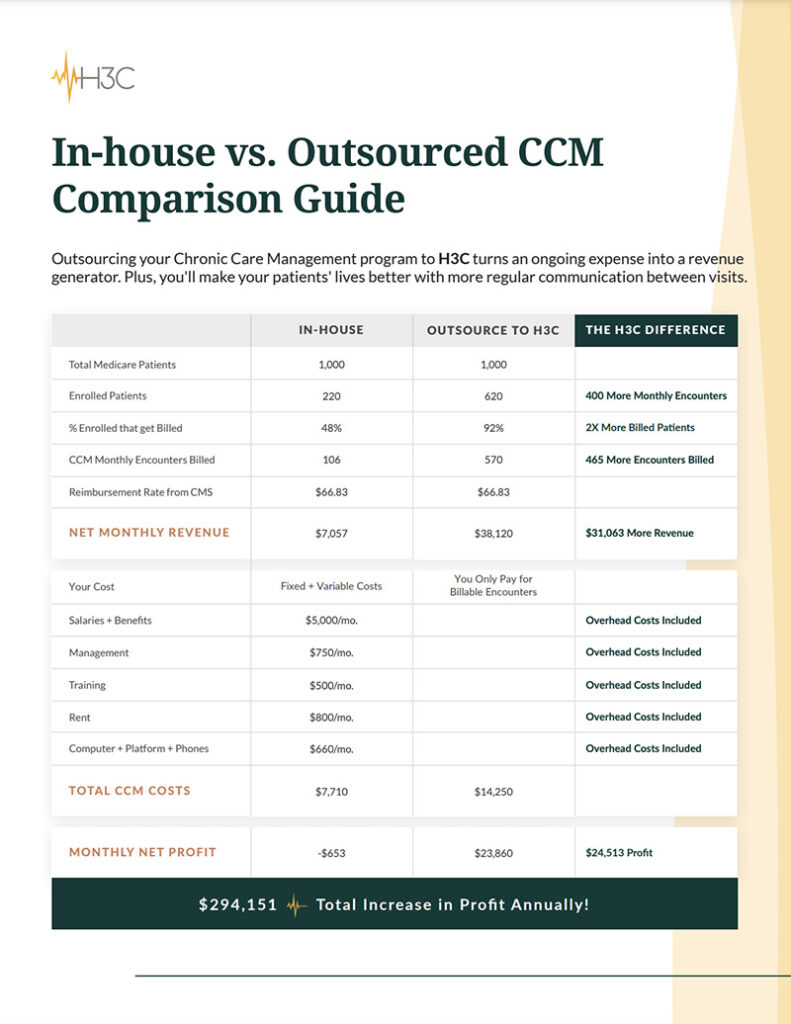
Spend Less Time Dealing With Codes. H3C Can Help.
At H3C, we help private clinics, RHCs, and FQHCs strengthen connections with more patients through high-quality, consistent CCM care—all while generating extra clinic revenue with minimal effort. Our 3-Step CCM process takes care of patient enrollment and outreach, personalized monthly check-in calls, and detailed reporting integrated directly into your existing EMR system in real time.
Our current clinic partners save significant staff time because:
- At the end of each month, we provide you with complete billing reports.
- Your custom billing report requires less than 30 minutes per month for a single staff member to submit for reimbursement from Medicare or private insurance.
- Every step of our process aligns with CMS compliance guidelines.
- We provide monthly risk stratification reporting so your staff can assess your Medicare population
at a glance.
Stop researching codes and start earning new revenue for your clinic while providing better patient care. Schedule a meeting to explore your risk-free, no-cost-to-start CCM program with H3C.