Table of Contents
As a leader in your organization, do you think monthly outreach with your most vulnerable population would help with patient satisfaction and outcomes? While your organization is doing all that it can, do you worry some patients might still fall through the cracks, unable to get the care they so desperately need? And now, some patients are too concerned about the risk of contracting COVID-19 to even make an appointment.
Chronic Care Management (CCM) services change the way you interact and care for your patients in the best way. When implementing chronic care management services, clinics experience improved patient engagement, which leads to better clinical results and an increased revenue stream. CCM is a way to meet the patient where they are, helping them invest in their healthcare.
What Is Chronic Care Management?
Chronic care management focuses on serving individuals on Medicare with two or more chronic conditions. CCM is a preventative service, helping your Medicare patients take a proactive approach to their health and wellness, while keeping them connected to their provider.
What does a Chronic Care Management Program Entail?
Help Manage Patient Conditions
Through a CCM program, patients work with your clinic to manage their chronic illness in a more consistent way. Monthly calls with your patients help identify changes to their health and navigate new challenges before you see them at their next appointment.
Stick with Patient’s Medicine and Treatment Plans
During monthly CCM calls, care coordinators encourage medication and treatment plan adherence recommended by the patient’s provider. This results in improved patient compliance and leads to happier, healthier patients.
Coordinate Care with Other Providers
CCM calls provide an opportunity to coordinate care with additional healthcare providers based on the patient’s needs identified in each call. If your patient’s health changes between appointments, you won’t need to wait until they visit the clinic to set up care with the appropriate medical team.
Are Chronic Care Management Programs Worth it?
In short, yes. Chronic Care Management programs pay off and lead to great patient care. On November 2, 2021, CMS announced its 2022 Medicare Physician Fee Schedule Final Rule, reinforcing the continued commitment to CCM Programs for providers and their beneficiaries. Inside the 2,400-page document is the announcement of a significant increase in reimbursement rates for CCM, Complex Chronic Care Management (CCCM), and Principal Care Management (PCM) services for FQHCs, RHCs, and Primary Care Organizations.
CCM services are eligible for reimbursements and must meet specific criteria, such as 20 minutes of dedicated patient time, patient-centric care plan development, and ongoing outreach to the participants.
The financial impact reinforces CMS’s commitment to the expansion of these programs and serves as further incentive for FQHCs and RHCs to implement these programs (if they haven’t done so already).
In 2022, G0511, the CPT code used by FQHCs and RHCs, will carry a reimbursement of $76.94 per encounter (per month), an increase of $11.70 or 18% over 2021 reimbursement levels.
The reimbursement rate for CPT code 99490 (the CCM look-alike code for non-FQHCs/RHCs) will also be increased in 2022 from $41.17 to $62.16, a year-over-year increase of 50%!
The financial impact of this change cannot be understated. For example, an FQHC with 1,000 patients enrolled in a CCM program where each patient received one phone call per month, would receive over $900,000 for one year of CCM services!
1 patient = $76.94
1,000 patients x 1 call per month = $76,940
$76,940 x 12 months
$923,280
in incremental reimbursements.
This level of incremental cash flow allows clinics to implement new patient programs, hire additional staff, and invest in resources that benefit your healthcare team and patients.
Benefits of a Chronic Care Management Program for Patients
Patients enrolled in a CCM program experience a closer connection with their healthcare provider and clinic through the service efforts. A CCM program not only improves patient engagement and compliance with a clinic, but it also gives your healthcare providers additional information on each enrolled patient, allowing them to see a broader picture of a patient’s current medical situation.
CCM patients are more likely to:
- Engage with the clinic and providers
- Have a higher rate of medication compliance
- Experience fewer hospitalizations
- Feel safe, resulting in a closer relationship with their doctor and clinic
The pandemic has made patients of all ages feel more comfortable connecting through remote outreach, making now an ideal time for your clinic to launch a chronic care management program.
Benefits of Chronic Care Management Programs for Providers
All healthcare facilities are running on tight budgets, limited resources, and overworked staff. It’s hard to imagine how adding more to the to-do list will help anyone. But a chronic care management service that is implemented correctly can not only provide valuable information to your healthcare team but also create a more streamlined approach to patient care.
A successful CCM program helps providers:
- Improve response time when issues arise through frequent contact with the patient, allowing your team to identify new developments in a patient’s health and pinpoint higher-risk patients.
- Pre-empt conditions that often result in acute-care circumstances.
- Connect to your patients, creating a more trusted relationship through monthly conversations empathizing and better understanding a patient’s healthcare challenges.
- Prevent acute situations by gathering more detailed information from your patients to discover health deficiencies by establishing a trusted relationship during monthly calls, allowing a patient to express concerns and ideas on their care.
- Increase revenue through CMS reimbursements, which leads to more budget for additional resources or staff to improve patient care.
Learn more about the simple, risk-free path to improving your patients’ care through our chronic care management services.
Chronic care management focuses on serving individuals on Medicare with two or more chronic conditions. CCM is a preventative service, helping your Medicare patients take a proactive approach to their health and wellness, while keeping them connected to their provider.
- Chronic Care Management gives caregivers and patients more control over their health and well-being, laying the foundation for healthier patient relationships and a higher quality of life.
- Chronic care management is one of the most effective approaches to improve the quality of life for patients with chronic illnesses. CCM services have been shown in studies to reduce depression, enhance social activity, and boost patient engagement in these individuals.
- Engage with the clinic and providers
- Have a higher rate of medication compliance
- Experience fewer hospitalizations
- Feel safe, resulting in a closer relationship with their doctor and clinic
- Improve response time
- Connect to your patients & build trust
- Gather more information about the patient
- Increase your revenue through CMS reimbursements
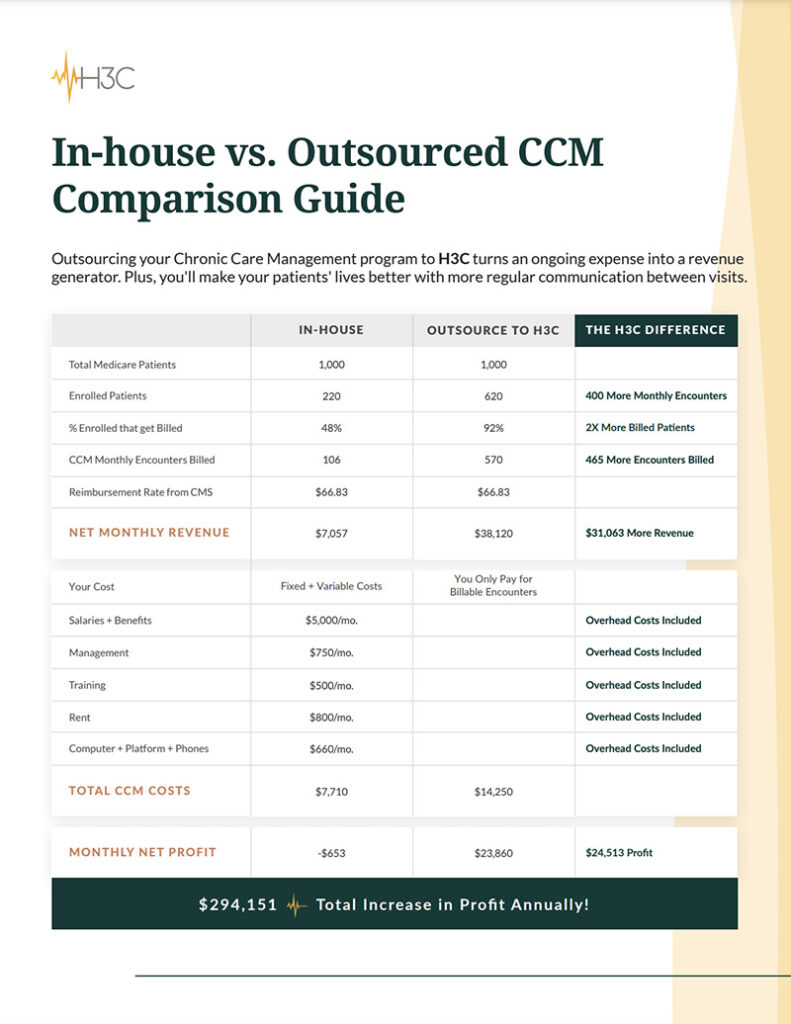
H3C is an innovative healthcare solutions company combining exceptional patient-centric care with cutting-edge technology. Working as an extension of your clinic, we provide chronic care management that helps improve patient experiences and outcomes while boosting both clinical value and revenue. Schedule a call and let’s discuss how we can help you.