Table of Contents
You’ve already determined that chronic care management (CCM) services would benefit your patient population. CCM programs change the way you interact with and care for your patients—improving patient engagement and health which leads to improved clinical results and an increase in revenue.
But what’s the best way to implement such a robust program into your clinic’s already demanding workflow?
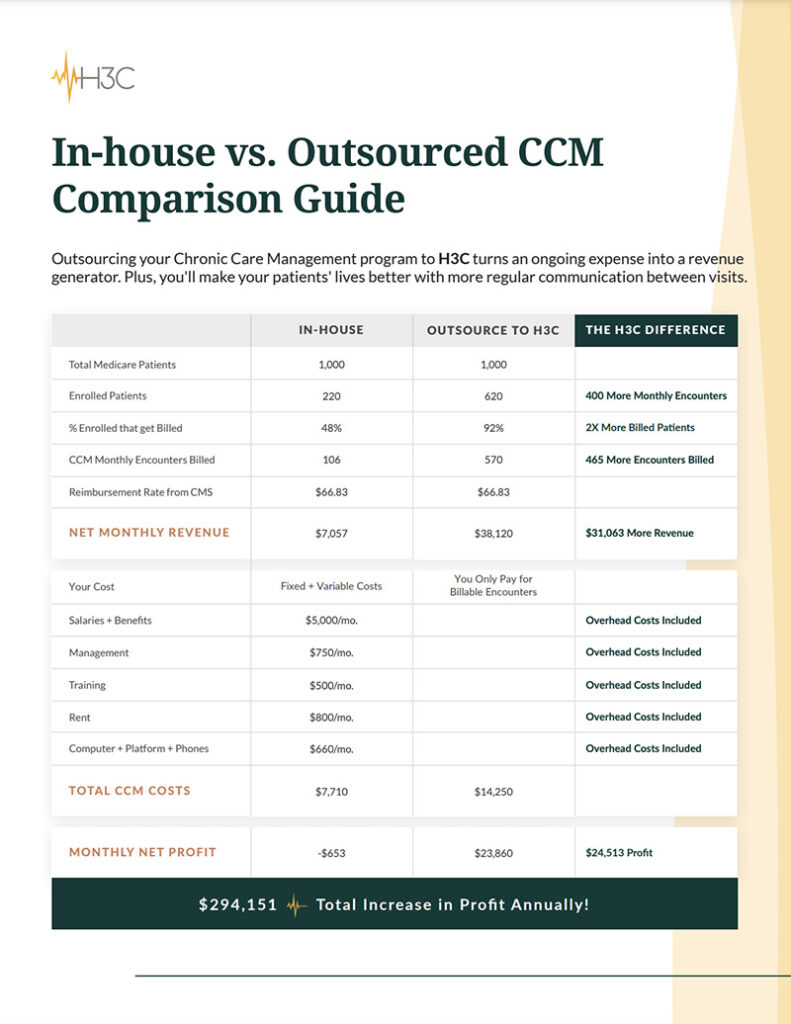
Federally qualified health centers and other clinics have two options to implement a CCM program. The first is to create and manage CCM services internally to meet the Medicare requirements necessary for the program. The second is outsourced chronic care management programs.
Some of those requirements include:
- An established care team managing the CCM program
- An extensive care plan for patients
- Communication and referral plan with clinical providers
- A minimum of 20 minutes per month of care coordination outside of appointments (not face-to-face)
The other option is to outsource the program to a third-party organization.
How to Manage Chronic Care Management Services Internally?
Managing a dynamic CCM program requires additional resources, staffing, and time to successfully improve patient care and submit reimbursements to Medicare. If your clinic has the capacity, there are many advantages to managing a CCM program internally.
Benefits of an Internal Chronic Care Management Program:
- Established connection with patients. Your clinic already knows your patients. You know who they are and what challenges they face. You don’t have to build trust with your patients because it’s already there.
- More control over the CCM program. When you outsource your CCM services, you need to trust that the company you hire is going to manage the program and represent your clinic in a way you see fit. By doing it internally, you have control over how patients are contacted and what is communicated with them. Plus, you won’t need to rely on an outside party to give you a detailed assessment of a patient’s health.
- No issues learning a new platform. By internally running the CCM services, your clinic won’t need to worry about implementing and learning a new platform that may or may not integrate into your EMR system and workflows.
- More reimbursement money. If you can manage the program internally, you don’t need to split the Medicare reimbursements with a third-party company or pay an additional fee for services. More money means more opportunity to expand your programs.
Before you can properly run a CCM program, you will need to make sure that you have the proper resources lined up in order to execute your plan. Adding these resources to your clinic costs money and takes time to research appropriate technology and train new staff. Learn more about whether your clinic is ready to launch a CCM program.
When Does Outsourcing Make Sense for FQHCs?
Before collaborating with a CCM provider, clinics need to properly vet any external partners to make sure they meet their expectations. When done correctly, externally sourced CCM services can provide much-needed relief to clinic staff while supporting patients’ healthcare needs.
Benefits of Outsourced Chronic Care Management Services:
- Implement a robust CCM program quickly. Internal implementation could take months to prepare but partnering with a CCM provider will only take a few short weeks. They already know what processes and technology need to be in place to get started and can help your team launch a CCM program as soon as possible.
- Relieve the administrative staff from additional strain. Hiring enough staff to internally support a CCM program puts a substantial amount of stress on the team of individuals tasked with launching such a program. Finding an external partner to supply the staff and resources needed takes a burden off your clinic’s plate.
- Additional help to care for your patients. Third-party organizations provide all the staff needed to enroll your patients, make monthly calls, document patient progress, and communicate with your team. Plus, some CCM companies will submit Medicare reimbursements for you!
- CCM services are their focus. And hopefully, like H3C, it’s all they do, making them well versed in how to manage a successful program.
- No upfront cost. Every clinic’s biggest concern is cost. Most CCM providers will not charge a service fee, but rather, split the reimbursement from Medicare with your clinic.
- Less time and effort from your staff. By utilizing a third-party’s resources, your staff has more time and energy to focus on caring for the patients in the office.
Partnering with a CCM provider seems like an easy decision, but not all third-party organizations are the same. There are a few cons to be aware of when evaluating potential partners.
Whether your clinic is considering an internal CCM program or is searching for a third-party organization to provide this service, there is no doubt that patients and clinics benefit from a successfully implemented and managed chronic care management program.
Whom can you trust to help support your patients’ care between clinic visits? Find out who helps clinics like yours care for their most vulnerable patient population with CCM services.
Chronic conditions that are expected to last at least 12 months or longer and put the patient at considerable risk of acute exacerbation, or functional impairment, are considered CCM. Examples could be:
- Alzheimer’s disease
- Arthritis
- Asthma
- Autism
- Cancer
- Cardiovascular disease
- Dementia
- Depression
- Diabetes
- Heart disease
- High blood pressure
- Hypertension
- HIV/AIDS
- Lupus
- Multiple sclerosis
The patient’s care team can bill for the time spent managing the patient’s conditions under CCM. This includes creating a thorough care plan, communicating and managing patients remotely such as over the phone, coordinating care amongst doctors, and managing medications.
Yes it can. For many physicians who do not have the professional staff bandwidth to provide continuing chronic care management, outsourcing solves the time-consuming CCM problem.
To create and manage CCM services internally, clinics need to meet the Medicare requirements necessary for the program. Some of those requirements include:
- An established care team managing the CCM program
- An extensive care plan for patients
- Communication and referral plan with clinical providers
- A minimum of 20 minutes per month of care coordination outside of appointments (not face-to-face)