Table of Contents
Well-constructed Chronic Care Management (CCM) programs are proven to not only improve patient care but can also provide additional revenue for clinics to help them expand or address areas of concern.
So how do you know if now is the right time to implement a chronic care management program in your clinic?
Ask yourself these questions:
- Do you have a growing Medicare population?
- Does your patient population have a subset of individuals with two or more chronic conditions?
- Do you have a qualified provider to oversee the program?
- Could you benefit from a dedicated team with time to contact your vulnerable patient population?
- Do you believe that monthly contact with patients with multiple chronic conditions can prevent more serious and/or more costly care in the long run?
If you answered, “yes” to these questions, now is the time to consider a CCM program to benefit your patients’ health and the quality of care at your clinic.
Did you answer “no”? Don’t leave quite yet! There are still ways for clinics with limited resources to implement a successful chronic care management program.
How Can a CCM Program Help Patients Facing Significant Health Challenges?
The national percentage of Medicare patients is projected to grow by 8 % each year through 2028. Many of these patients are managing – or not managing – two or more chronic conditions, putting them at high risk of falling through the cracks between appointments or worse – hospital stays. As this patient population continues to grow, your clinic is faced with more individuals struggling to get the care they need and deserve.
With a successful CCM program, clinics can help address care plan and medical treatment questions as well as identify any serious changes to a patient’s health. Staying in touch with your vulnerable patients can proactively help reduce the risk of hospitalizations among this population through consistent communication that builds trust with their clinic and providers.
Do You Have the Right Resources to Implement a CCM Program?
There are plenty of reasons to start a CCM program, but it’s not as simple as saying, “ready, set, go!”
To develop a successful CCM program for your patients, it’s important to make sure you have the resources needed before jumping in. This is especially important to ensure Medicare guidelines are being met in order to receive payment for your chronic care management program.
Some of those requirements include:
- An established care team managing the CCM program
- A comprehensive CCM care plan for patients
- Communication and referral plan with clinical providers
- A minimum of 20 minutes per month of care coordination outside of appointments (not face-to-face)
These requirements and the demands of a CCM program take additional staff, time, and attention in order to have a positive impact on patients.
For every 1,000 patients, you need:
- Six individuals making calls and assessing patients
- One RN to oversee callers
- One Director of Operations to oversee the processes
- One clinical lead to communicate concerns and updates on each patient and demographic
- The right technology: a call-center platform, an assessment program, and a work organizer
If your clinic has all these things, you’re ready to start helping your chronically ill patients.
Move Forward with a Chronic Care Management Partner
If you’re like most clinics, you don’t have all those resources lined up and ready to go. And you probably don’t have the budget to hire the extra staff needed to call and assess patients and manage a program.
Even though you may lack internal resources, it doesn’t mean you can’t provide a CCM program to your patients. Partnering with a company that focuses on chronic care management is one way to give your patients the exceptional care they deserve, while also providing valuable information to your clinic that can lead to improved patient care.
What to Look for in a Chronic Care Management Partnership
Not all CCM programs are the same. You want a partner that will operate within your workflow and clinic processes, streamlining the new program easily into your current day-to-day operations.
Here’s what you need to look for when choosing a CCM provider:
- Allows you to connect with patients between visits. A CCM provider should communicate with patients every month, helping them feel cared for and connected to their providers between visits.
- Creates an exceptional, customized, patient experience. Their program should be easy for your patients to understand and enroll, and they should find value in their monthly conversations with care coordinators. This way, more patients remain in the program and feel better connected to both the CCM team and their provider.
- Enrolls a high percentage of your multi-chronic Medicare population. The idea behind a CCM program is to help the patients become more accountable for their own health. Armed with regular “check-ins” and data, your internal staff can risk stratify your population and reserve their time for the patients that need help the most.
- Requires no new software. You want to look for a partner that can easily integrate with your clinic’s own EMR system, providing data and insights in real time without the need for third-party software or plug-ins.
- Provides quality reporting and insights. Your CCM provider should provide your healthcare team with data that will help them quickly spot issues and identify patients at greater risks through comprehensive, high-quality reporting and analytics.
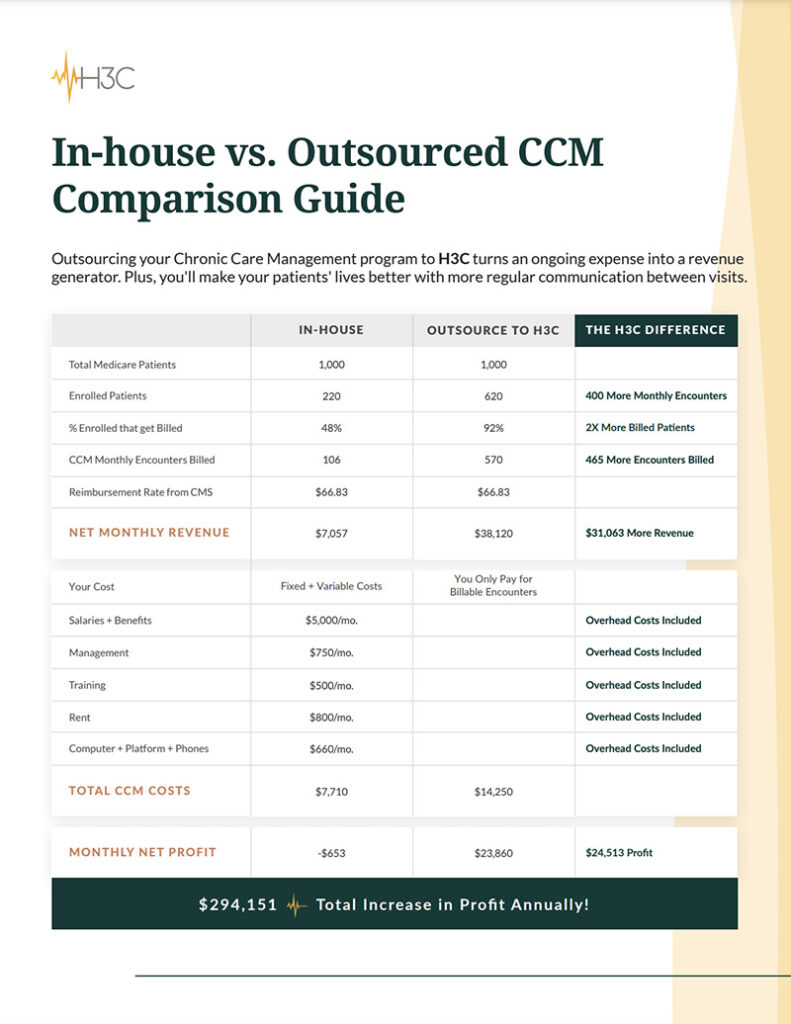
- Increases revenue and clinic resources. With the right partner, your clinic should be able to use the revenue gained from the CCM program to hire more staff, build more programs and
provide more solutions to your patients.
Is your clinic ready to implement a CCM program?
If your clinic needs help to start a chronic care management program, there are plenty of resources available to get started. Learn more about the simple, risk-free path to improving your patients’ care. Schedule a call with a CCM expert at H3C.
Chronic care management is care coordination services done outside of the regular office visit for patients with multiple (two or more) chronic conditions expected to last at least 12 months or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. These services are typically non-face-to-face and allow eligible practitioners to bill for at least 20 minutes or more of care coordination services per month. (CMS)
With a successful CCM program, clinics can help address care plan and medical treatment questions as well as identify any serious changes to a patient’s health. Staying in touch with your vulnerable patients can proactively help reduce the risk of hospitalizations among this population through consistent communication that builds trust with their clinic and providers.
It is important to ensure Medicare guidelines are being met in order to receive payment for your chronic care management program. Some of those requirements include:
- An established care team managing the CCM program
- A comprehensive CCM care plan for patients
- Communication and referral plan with clinical providers
- A minimum of 20 minutes per month of care coordination outside of appointments (not face-to-face)
Here’s a list of what you need to look for when choosing a CCM provider:
- Allows you to connect with patients between visits
- Creates an exceptional, customized, patient experience
- Enrolls a high percentage of your multi-chronic Medicare population
- Requires no new software
- Provides quality reporting and insights
- Increases revenue and clinic resources
H3C is an innovative healthcare solutions company combining exceptional patient-centric care with cutting-edge technology. Working as an extension of your clinic, we provide chronic care management that helps improve patient experiences and outcomes while boosting both clinical value and revenue. Schedule a call and let’s discuss how we can help you.