Chronic care management (CCM) is a preventative service provided to individuals who live with two or more chronic conditions. CCM is covered by Medicare and offered by clinics to help increase patient interactions with their provider in order to achieve better health and wellness outcomes. From Alzheimer’s to asthma, arthritis to diabetes, there are many different types of chronic conditions that depend on diligent care plans to prevent escalation.
In order to be eligible for a chronic care management program, a patient must meet the criteria set by Medicare. It can sometimes be difficult, however, to get a consistent answer about all the conditions that qualify. In this blog post, we will explore what an eligible chronic condition is, and who qualifies as having one.
What Qualifies as a Chronic Condition for CCM?
The Centers for Medicare & Medicaid Services broadly define a chronic condition as an illness or ailment that lasts 12 months or more and requires ongoing medical attention or limits activities of daily living. Common examples of chronic conditions include:
- Diabetes
- Heart disease
- Arthritis
- Cancer
- Alzheimer’s disease
- Kidney disease
See more common, eligible chronic conditions in our Ultimate Guide to CCM.
According to the Agency for Healthcare Research and Quality, which sponsors the Healthcare Cost and Utilization Project’s (HCUP) Chronic Condition Indicator (CCI) database, there are approximately 12,500 conditions designated as chronic.
H3C uses the CCI database from the HCUP to identify eligible chronic conditions because it is the most authoritative resource. Unfortunately, your Electronic Medical Record system provider may not be using this best practice.
David Vana, Chief Information Officer at H3C, said, “We have occasionally run into issues with certain EMRs (most commonly eClinicalWorks) that don’t properly recognize the standard list of chronic conditions as identified by HCUP. To resolve this, H3C provides our clients the complete list of chronic conditions so they may update their EMR.”
Who Qualifies for Chronic Care Management Services?
For an individual to qualify for CCM services, the following criteria must be met:
- The patient must be on Medicare and face at least two chronic conditions.
- The chronic conditions are expected to last at least 12 months.
- Patients have consented to be in the CCM program.
- The patient has received an individualized care plan.
- Clinical time spent with enrolled patients must be at least 20 minutes and go up to 60 minutes.
According to the American Academy of Family Physicians, in-house CCM services can be provided by a variety of clinic staff, but only one physician or other qualified healthcare professional can bill for CCM services per patient per calendar month. This can include a physician, clinical nurse specialist, nurse practitioner, or physician assistant.
Why Are Chronic Care Management Services Important?
While many patients with multiple chronic conditions can manage their health systems with the right treatment and prescriptions, their quality of life typically depends on strict, consistent adherence to their care plans, which is challenging for many.
Patients enrolled in a CCM program experience improved patient engagement, stronger connections to their doctor and clinic, and a higher rate of medication compliance. This helps reduce hospitalizations, visits to the emergency department, and the long-term cost of healthcare.
On the clinic side, a successful CCM program provides enhanced insights into patients’ lives and conditions, which helps providers:
- More quickly identify new developments in a patient’s health
- Pre-empt conditions that often result in acute care circumstances
- Build a stronger, more trusted relationship with patients through monthly conversations
How Outsourcing CCM Services to H3C Can Help You
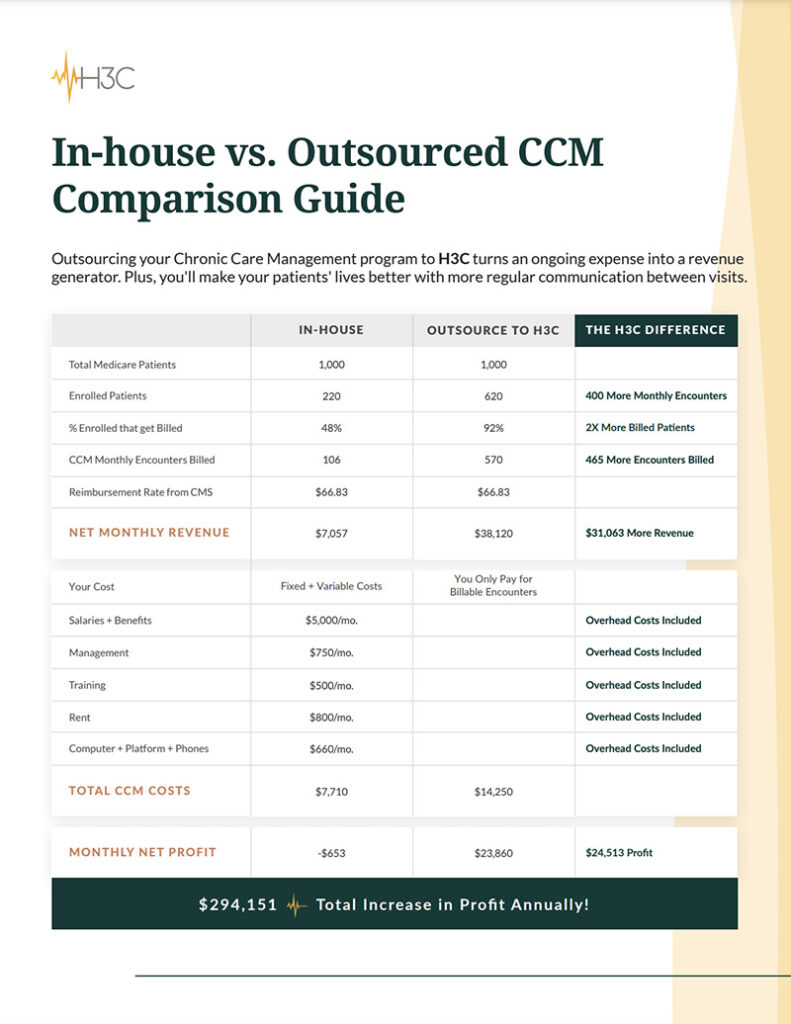
If you have ever considered a CCM program, you know that the easy part is recognizing the value for your patients and clinic. The hard part—and the roadblock for many clinics—is the enormous strain on staff time to build a program in-house.
At H3C, we use a clear three-step process that has helped many of our provider partners reach full implementation in just weeks, without hiring or capital expenses:
- Step 1: We help you identify eligible patients and take care of all the outreach to inform them of the CCM program opportunity.
- Step 2: Each enrollee receives a monthly phone call from their dedicated H3C representative who understands their current medical challenges and tendencies.
- Step 3: We integrate reporting and patient assessments directly into your existing EMR system in real time. In-office visits become more productive and beneficial for the patient and the provider, and no extra staff time is spent learning new technology.
The cost of working with H3C?
We provide our CCM program and technology at no cost to clinics. And, at the end of each month, we provide complete billing reports to help you easily submit for Medicare reimbursements and generate additional revenue from offering CCM services.
Come learn why clinics like yours trust us to provide top-level CCM care for their patients. Discuss your patients’ needs with CCM specialist, Pete Desjardins, at H3C today.