Table of Contents
Running a CCM program in-house is a resource-heavy undertaking. Staffing, tracking systems, enrollment and compliance all present unique obstacles. Outsourcing is not without concerns either and clinics must hunt hard to find a trusted partner willing to act as an extension of the team.
Making the decision to pool resources internally vs. outsourcing is a major consideration that requires a deep dive into the multiple layers of effective CCM programs. At the end of the day, clinics should choose an approach that provides patients with the highest level of care while delivering excellent chronic condition management between visits.
What do you need to implement chronic care management services in your FQHC?
The resource load is significant and you will find a long list of questions developing while planning an in-house CCM program. These are just a few high-level questions to get started:
- How will we hire and train new staff?
- What enrollment pathways are needed (aside from case management)?
- How is CMS compliance managed with detailed documentation and recording?
- Which time management mechanisms are needed?
- What are the start-up costs?
- How much overhead is added to quarterly clinic expenses?
Expanded Personnel Resources
Staffing presents the first challenge and ranks high among the most difficult aspects of any program. Nurses are maxed out on work and adding specialized staff to manage FQHC CCM clinic caseloads is an absolute necessity.
New staff members require in-depth training, adding to the overhead. The CCM program will have a wait period to launch while each member is sourced and trained through processes to ensure compliance is met and quality management is delivered from day one.
Attempting to overload nurses with CCM tasks creates a scenario where day-to-day details slip through the cracks. Nurses need every minute to focus on cases and direct patient care. Running calls and checkups requires a new staff segment that can interface with nurses as needed.
CMS Compliance and Implementation
After staffing the clinic, training and implementing CMS Compliance processes is critical. How will your clinic record and document patient interactions to maintain compliance? Weighing the pros and cons between building an internal system or incorporating an external software management system for compliance is a necessary internal conversation.
External systems involve onboarding for new software and additional training for current staff and new hires. Internal management systems mean a project lead will be hired or contracted to develop compliance systems. Both are time-consuming to implement.
Tracking Systems and Enrollment Pathways
Effective Chronic Care Management is a hands-on job that benefits from a systematic approach with focus on preventative needs and real-time response. In CCM, preventative management executes strategic Q&A where asking the right questions reveals patient needs that ultimately help identify vulnerabilities requiring scheduled or immediate care.
How will your internal team:
- Determine which metrics and conditions you will track?
- Process questions to ask against specific conditions?
- Develop internal processes, tracking and management systems?
Managing a diabetic patient is different from a cancer patient who is different from a rheumatoid arthritis patient. Each condition requires specificity in the conversation to really understand and connect with the patient’s needs.
In-house chronic care management is time intensive from every perspective. Finding the balance between efficiencies in terms of process while dedicating time to individual patients takes time and experience to develop and execute with consistency.
Will Your Clinic Need a Dedicated Enrollment Team?
Physician enrollment doesn’t translate for internal CCM programs. They are simply too busy and focused on care to take on the administrative enrollment tasks associated with CCM. It’s not a good use of their valuable time and the need for an enrollment team quickly becomes apparent.
Enrollment teams manage the initial discovery, patient interviews, waivers, documentation and file setup for management moving forward. They qualify patients, document background and bring patients into the system where they are moved into checkups, prescription fills and regular calls for the preventative conversations and management that ultimately save nurses and staff time on the floor.
Pulling together resources and forming this team is time intensive and can take a year before everything is running. Can your clinic wait for the launch while eating the overhead? Running the costs and wait times is an important consideration for clinic leaders.
The Challenges of Finding a Trusted Partner
While some clinics will benefit from an in-house program, many cannot afford to wait and invest massive amounts of time in training, new infrastructure and program development. Focusing on immediate patient care is top priority.
A trusted partner can excel at CCM, ensuring patients get the care needed between each visit.
But how do you identify the right partner?
- Whom will you trust to talk to your patients?
- Are they calling regularly and really connecting (not just getting to billable status)?
- Can it work inside my own EMR in real time? (No third-party software setup – we integrate.)
- How much clinic time is required? Very little.
- Is it cost-effective? Cost-effective – no startup, no lengthy contracts (add cost analysis).
Quality CCM partners act as an extension of your team and provide a support system that empowers nurses to focus on caseloads without getting in the weeds on CCM tasks.
The H3C CCM program:
- Prioritizes patient needs above all else.
- Invests significant call times for every patient.
- Works inside the existing EMR. No third-party software required.
- Requires no clinic time to manage.
- No startup costs or lengthy contracts.
- Manages compliance, enrollment and all admin.
H3C is built to shoulder the weight of CCM through specialization that ultimately delivers immediate profit to the clinic and care benefit to the patients and staff. Monitor the pulse of your most vulnerable patients with the H3C difference.
According to CMS: Chronic care management is care coordination services done outside of the regular office visit for patients with multiple (two or more) chronic conditions expected to last at least 12 months or more, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. These services are typically non-face-to-face and allow eligible practitioners to bill for at least 20 minutes or more of care coordination services per month.
The resource load is significant and you will find a long list of questions developing while planning an in-house CCM program. These are just a few high-level questions to get started:
- Expanded Personnel Resources
- CMS Compliance and Implementation
- Tracking Systems and Enrollment Pathways
A trusted partner can excel at CCM, ensuring patients get the care needed between each visit. There are a few questions you need to ask beforehand:
- Whom will you trust to talk to your patients?
- Are they calling regularly and really connecting (not just getting to billable status)?
- Can it work inside my own EMR in real time? (No third-party software setup – we integrate.)
- How much clinic time is required? Very little.
- Is it cost-effective? Cost-effective – no startup, no lengthy contracts (add cost analysis).
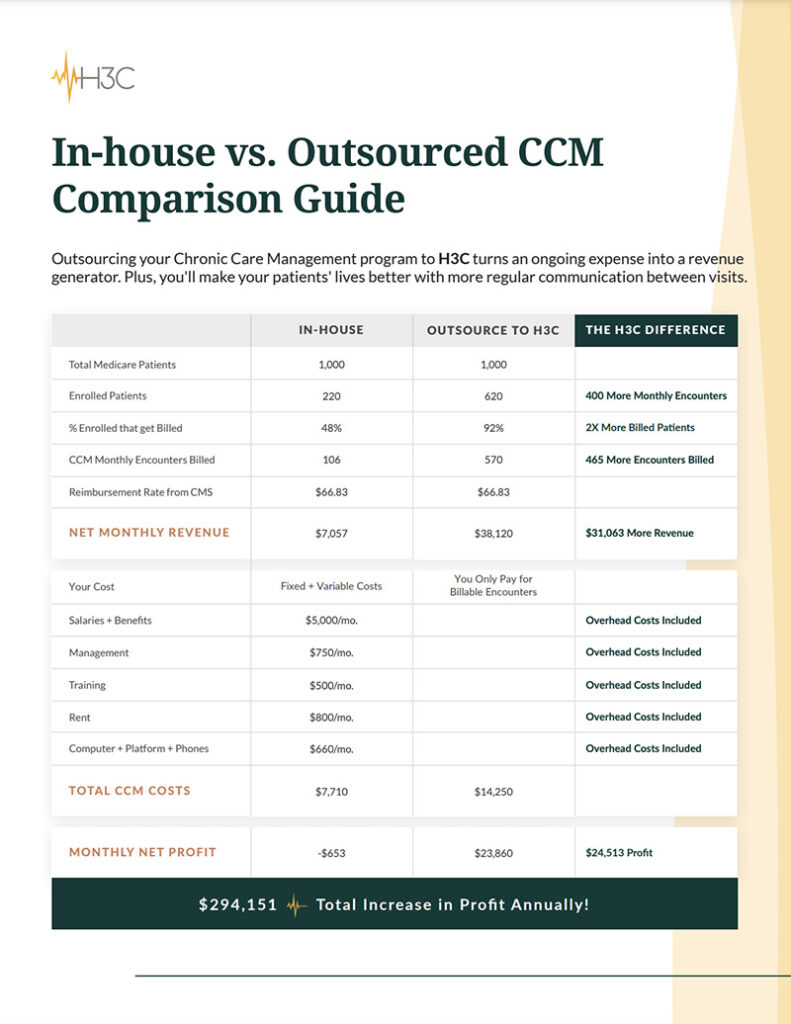
Outsourcing can work effectively in this manner but clinics can also benefit from working with a partner on a mixed model to maximize patient reach, control, and resourcing across the internal and external teams. Learn more about in-house vs. outsourced chronic care management, here.
H3C is an innovative healthcare solutions company combining exceptional patient-centric care with cutting-edge technology. Working as an extension of your clinic, we provide chronic care management that helps improve patient experiences and outcomes while boosting both clinical value and revenue. Schedule a call and let’s discuss how we can help you.