Table of Contents
Case management is imperative to every clinic and FQHC, allowing you to effectively care for the sickest individuals in your patient population. If you already oversee a case management program, you might not think you need to add chronic care management (CCM) services to your clinic. However, CCM programs are not only proven to improve patient care, but they actively support case management programs within the clinic.
To better understand the difference between care management vs case management, let’s dive deeper into the details of each program.
What is Case Management?
Case management programs focus on patients with acute conditions.
These individuals have:
- Frequent hospitalizations and emergency department visits
- Multiple conditions to manage, including some severe illnesses
- Complex needs that take the full focus of the case manager and program
Case management services focus on the sickest patients, about 5-10% of the Medicare population, and concentrate on managing acute episodes of a specific disease.
What does Case Management Services include?
The goal of case management is to address and prevent further progression of the disease. Case management programs accomplish this by:
- Requiring thorough assessments of each patient prior to acceptance in the program, including evaluation of medical, financial, and legal issues
- Monitoring patients through hands-on assessments like vital signs
- Utilizing certified case managers, with a background in nursing or social work
- Providing value-based care that has been shown to reduce overall healthcare costs by improving patient outcomes, even though it does not qualify for Medicare reimbursements
Case management is critical to every healthcare system that desires to best serve its patient population. However, it takes a lot of resources to focus on a small percentage of the population and their severe needs.
What is Chronic Care Management?
Where case management programs only focus on the sickest patients, CCM programs concentrate on the rest of the Medicare population with two or more chronic health conditions. CCM is a preventative service, helping your at-risk patients take a proactive approach to their health and wellness while keeping them connected to their providers.
What do CCM Services include?
Through a CCM program, patients work with your clinic to manage their chronic illness in a more consistent way. CCM services help clinics:
- Enroll patients with two or more chronic conditions
- Monitor patients through monthly phone call assessments
- Identify and report changes or issues in a patient’s health to their team of healthcare professionals
- Designate staff internally or through a third-party provider
- Qualify for Medicare reimbursements
How Do Chronic Care Management Services Support Case Management?
It’s not a question of whether your clinic should implement a case management program OR CCM services. Instead, you should focus on how CCM services can improve and support a case management program at your clinic. With patients enrolled in a CCM program, your clinic will see fewer of these individuals needing case management services in the near future.
Preventative Care with CCM
CCM programs are designed to help individuals with multiple chronic conditions manage their care and follow their treatment plans. The service strives to keep patients on the path of improving their health by providing preventative-focused assistance.
A quality CCM program supports Case Management by:
- Identifying any issues or changes to health prior to becoming a serious incident needing hospitalization
- Improving patient health with fewer hospitalizations and more adherence to treatment and medicine plans, prolonging their ability to avoid a case management program
- Alleviating case management programs from becoming overwhelmed by acutely ill patients through preventative care measures
Through the implementation of a CCM program, your clinic can provide more attentive care to case management patients who are at a higher need of services.
How CCM Services Benefit Your Clinic?
CCM services are managed internally or through a third-party organization. Regardless of how your program is set up, a successful CCM program can provide significant benefits to patients and to your healthcare professionals.
Quality CCM programs support healthcare clinics and their staff by:
- Keeping patients connected with their clinic and healthcare professionals between appointments, and increasing patient engagement through monthly conversations
- Offering more time for staff to focus on face-to-face interactions during appointments instead of splitting their attention between calling patients and clinic visits
- Lightening the burden of identifying issues in every patient through monthly assessments
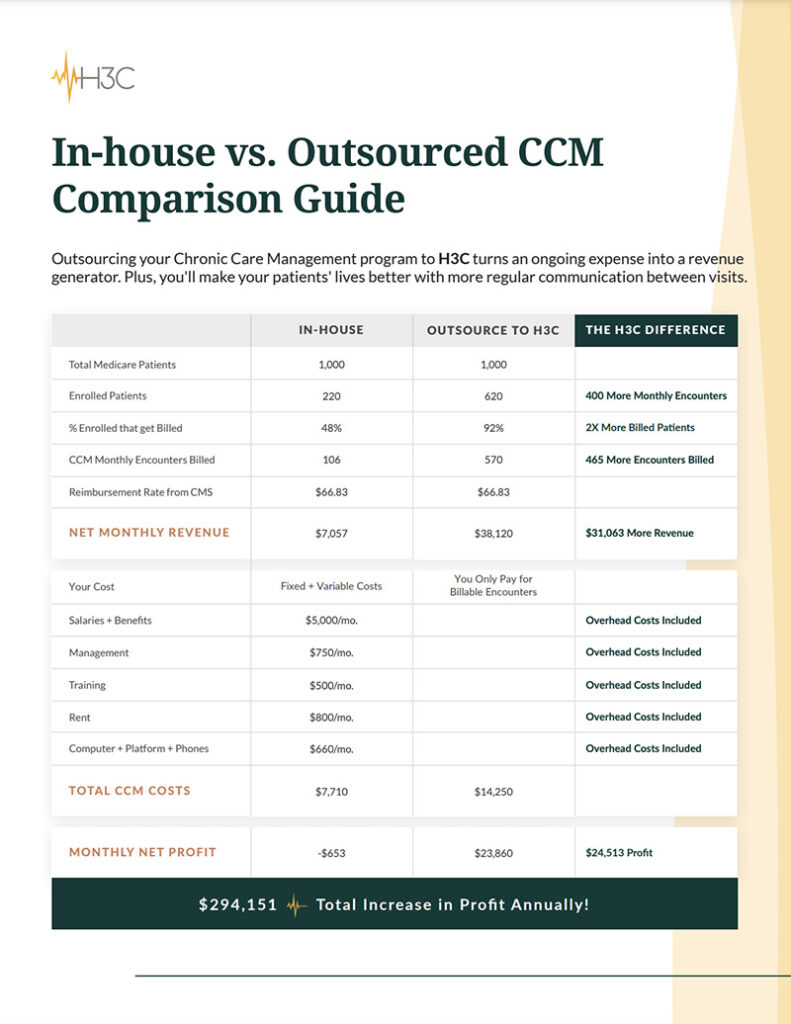
- Increasing revenue through CMS reimbursements, which leads to more budget for additional resources or staff to improve patient care
Want to learn more about the benefits of implementing a CCM program at your clinic? Learn more about how your clinic and patients can benefit from CCM programs.
CCM programs concentrate on Medicare patients with two or more chronic health conditions that are expected to last for 12 months or longer.
Case management services focus on the sickest patients, about 5-10% of the Medicare population, and concentrate on managing acute episodes of a specific disease.
Case managers frequently collaborate with doctors, social workers, families, and human service providers. Case managers help patients by:
- Assessing their needs
- Reviewing treatment choices
- Developing treatment plans
- Coordinating care
- Tracking their progress
- Thorough assessments of each patient prior to acceptance in the program, including evaluation of medical, financial, and legal issues
- Monitoring patients through hands-on assessments like vital signs
- Value-based care that has been shown to reduce overall healthcare costs by improving patient outcomes, even though it does not qualify for Medicare reimbursements
A quality CCM program supports Case Management by:
- Identifying any issues or changes to health prior to becoming a serious incident needing hospitalization
- Improving patient health with fewer hospitalizations and more adherence to treatment and medication plans, prolonging their ability to avoid a case management program
- Alleviating case management programs from becoming overwhelmed by acutely ill patients through preventative care measures
Case management programs only focus on the sickest patients, CCM programs concentrate on the rest of the Medicare population with two or more chronic health conditions.