Table of Contents
Patient satisfaction has been emerging as a paramount focus in the healthcare industry. Starting back in 2006, hospitals and health clinics began measuring patient satisfaction through the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS. The scores from this assessment hold significant influence over reimbursement rates and the overall financial success of healthcare organizations. They also serve as a key indicator of quality in the eyes of the community and patient population.
The challenges facing healthcare organizations right now are connected: lagging revenue and low patient satisfaction in this post-pandemic world. Often, there is not enough financial flexibility to hire more staff and fund the new programs that would contribute to improved patient satisfaction. This perpetuates a cycle of financial strain and diminished ratings.
Recognizing the role HCAHPS scores play in clinic revenue, it’s clear that hospitals and health systems need a new solution. In this blog post, we will explore how a chronic care management (CCM) program may be the best strategy for improving patient satisfaction – and increasing revenue.
What Are HCAHPS Scores?
HCAHPS scores are standardized survey measures used to evaluate and compare the quality of care delivered by hospitals across the U.S. These surveys are randomly administered to discharged patients, capturing their perspectives on various aspects of care received during a specific visit. The surveys delve into key areas of assessment, including:
- Communication with healthcare staff
- Responsiveness of hospital staff
- Cleanliness
- Quietness
- Pain management
- Discharge information
The resulting scores from these surveys provide valuable insights into patients’ perspectives and experiences. They allow hospitals to identify areas for improvement and track their performance over time.
Why Do HCAHPS Scores Matter?
In addition to identifying internal areas of improvement, HCAHPS scores are publicly reported to help patients make informed decisions about their healthcare providers. This gives HCAHPS scores significant influence over three important objectives:
- Attracting new patients
- Public perception and community reputation
- Reimbursement rates from government payors
How HCAHPS Scores Influence New Patients
Positive HCAHPS scores signal to potential patients that the hospital or clinic prioritizes patient satisfaction and delivers excellent care. Higher scores are indicative of positive patient experiences, including effective communication, responsive staff, and quality outcomes. Hospitals with higher HCAHPS scores instill confidence and trust, ultimately contributing to reputation and growth.
How HCAHPS Scores Influence Public Perception
Similarly, a hospital with consistently high scores earns a reputation from its community for delivering exceptional patient-centered care. This can garner trust and pride within the community. Negative scores, on the other hand, may lead to a loss of public confidence or potential negative media coverage. Hospitals with stronger HCAHPS scores are more likely to strengthen their bottom line by fostering community trust and support.
How HCAHPS Scores Influence Clinic Reimbursement Rates
HCAHPS scores impact hospital reimbursements through the Hospital Value-Based Purchasing (VBP) Program. Under the VBP program, a portion of Medicare reimbursement payments to hospitals is tied to their performance on quality measures, including HCAHPS scores. Higher-performing hospitals with better HCAHPS scores receive positive reimbursement adjustments, leading to increased Medicare payments.
Chronically Ill Patients Play a Big Role in Your HCAHPS Score
Patients with chronic conditions represent a critical population due to their significant dependence on healthcare services. Findings from this study highlight the substantial impact of chronic conditions on hospital admissions. In 38% of cases, a chronic condition was the primary reason for hospitalization. As a result, the chronically ill population exerts a disproportionate influence on the HCAHPS scores of your hospital or health system.
This population also often requires care across multiple care sites. With all the benefits of connected care, a notable challenge lies in the difficulty of distinguishing between individual providers or interactions.
A white paper published by the American Hospital Association (Page 23) highlights a disconnect that can arise when a patient’s doctor schedules a pre-op appointment, for example. The patient’s expectations after a conversation with their doctor may not align with the hospital’s practices. Despite concerted efforts to bridge provider gaps and ensure continuity of care, the existing siloed approach may not adequately capture the true patient experience.
Recognizing and addressing the unique needs of chronic care patients is essential for improving HCAHPS scores and overall care quality. This group relies on good communication and consistent experiences from hospital to doctor to home care.
How a CCM Program Can Improve HCAHPS Scores
A well-executed chronic care management program can support the needs of your chronically ill patient population and move the needle on your HCAHPS scores.
For example, hospitals and health systems that want to improve their patient satisfaction scores are advised to focus on the following composite areas:
- Doctors’ communication with patients
- Nurses’ communication with patients
- Hospital staff responsiveness
- Pain management
- Medication communication
- Discharge information communication
- Care transition
A CCM program can positively influence five of these seven major components through enhanced patient communication, care coordination, proactive monitoring, preventative care, and patient education.
Enhanced communication and care coordination: When enrolled in a CCM program, patients are assigned dedicated care coordinators. This enables patients to receive personalized support, leading to more consistent communication between healthcare providers. Coordinated care also supports seamless transitions between different care settings, such as hospitals, clinics, and home care. Clear, timely communication within a CCM program helps address patient concerns and positively influences HCAHPS scores.
Proactive health monitoring and preventative care: CCM programs place a strong emphasis on proactive health monitoring and preventative care. By closely monitoring medication adherence and chronic condition management after hospitalization, CCM programs can identify and address potential issues before they escalate. This continuity of care leads to better patient outcomes, reduced hospitalizations, and improved HCAHPS scores.
Patient education and empowerment: CCM programs also prioritize patient education regarding lifestyle modifications, medication adherence, and treatment plans. CCM can reinforce and recommunicate discharge information, assist the patient with care transition instructions, and even make follow-up appointments for them. Patients who feel well-informed are more likely to experience optimal outcomes and provide positive feedback on HCAHPS surveys.
Start Now With an Outsourced Chronic Care Management Program
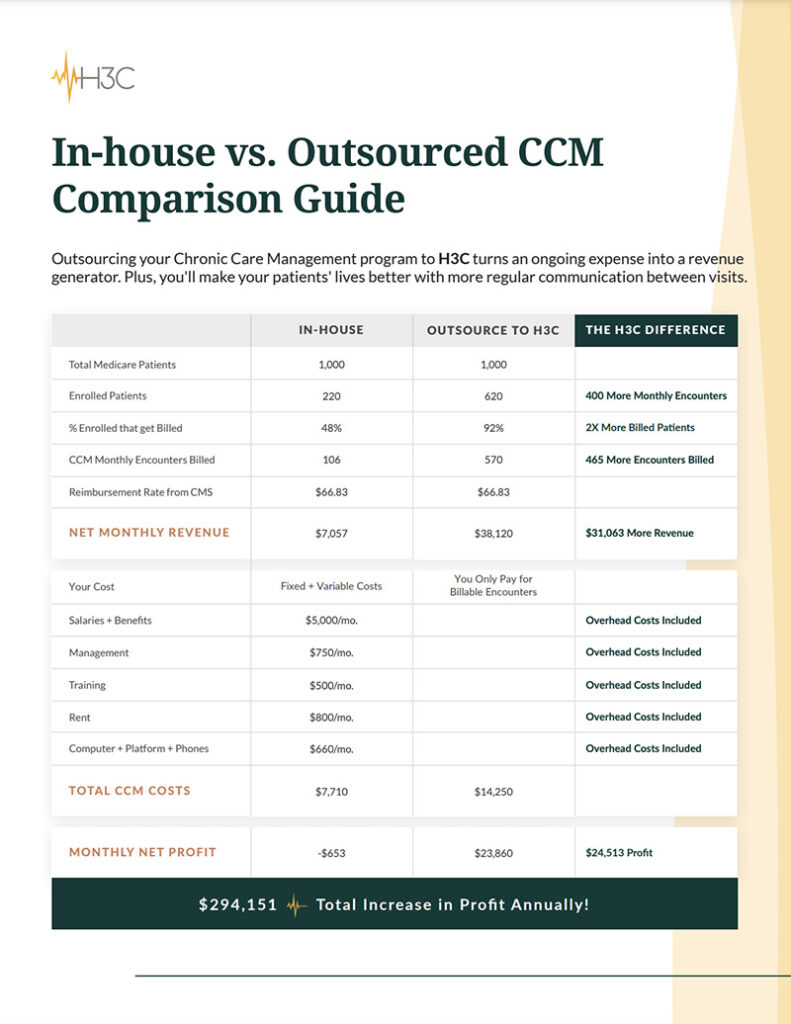
CCM programs change the way you interact with and care for your chronically ill patients. When done correctly, outsourced CCM services can provide much-needed relief to staff, support patients’ healthcare needs and drive increased reimbursement revenue. With H3C, you can launch your CCM program in just a few short weeks. Best of all, there are no additional costs to your hospital or health system or time lost for staff training.