Table of Contents
In the ever-evolving landscape of healthcare, physicians and clinics face the vital challenge of providing seamless, comprehensive care for patients. This is especially important for highly vulnerable chronic-care patients.
Healthcare continuity and coordination have emerged as fundamental aspects of quality healthcare delivery, with profound implications on patient outcomes.
Studies have shown that patients who experience seamless continuity of care have better healthcare outcomes and are more satisfied with the treatment they receive.
What is meant by continuity of care?
Continuity of care refers to the consistent and uninterrupted delivery of healthcare services to individuals over time. It emphasizes an ongoing relationship and clear communication between patients and their healthcare team.
Continuity of care has been found to reduce mortality rates, lower the use of hospital care, decrease overall healthcare costs and improve patient adherence to medical advice.
What is meant by coordination of care?
Coordination of care refers to effective communication, collaboration and shared decision-making between different healthcare providers and settings. This ensures that all aspects of a patient’s care align and work together seamlessly, which improves the quality and efficiency of care.
The Challenge Facing Clinics
While coordinated, comprehensive care is key to better patient outcomes and satisfaction, implementation has proven difficult. Clinics are understaffed and overburdened. There is little time to learn the technology required or parse through records to see which patients are most at risk.
How a CCM Program Can Help?
A chronic care management (CCM) program is a comprehensive approach to managing and coordinating care for patients who are on Medicare and have two or more chronic conditions. CCM is a preventative service that provides ongoing support, education and monitoring to improve patient outcomes while keeping them connected to their provider.
A well-run CCM program naturally facilitates continuity and coordination of patient care. It is a crucial tool for healthcare teams and systems to deliver top-notch care and optimal patient outcomes in several ways:
- Eliminate disjointed care
- Provide seamless communication
- Decrease costs for financially vulnerable patients
- Drive new clinic revenue
Let’s take a closer look at each.
- Eliminate Disjointed Care
A coordinated healthcare model reduces inefficiencies and the chances of patients experiencing siloed care from providers who are not in sync. Disjointed care can lead to duplicate testing, delayed treatment, confusion for patients and their families, and poorer overall outcomes. Care coordination, such as a CCM program, can play a pivotal role in eliminating disjointed care by fostering seamless collaboration among healthcare providers.
A CCM program establishes a centralized point of contact, typically a care coordinator, who oversees the patient’s care journey. This dedicated coordinator ensures that information is effectively shared among providers and facilitates smooth transitions between different healthcare settings.
- Provide Seamless Communication
Seamlessly sharing detailed patient information among all involved clinical teams results in a better patient experience. This is possible by reducing redundant office visits and increasing confidence in the care plan. This cohesive approach improves adherence to the care plan and enhances treatment outcomes for patients.
A coordinated care model facilitated by a CCM program creates a collaborative environment where providers share pertinent patient information, care plans, and urgent updates in a timely manner.
- Decrease Costs for Financially Vulnerable Patients
When care is coordinated, patients are less likely to experience complications or deteriorating conditions, which minimizes additional healthcare costs. Especially for patients who are on Medicare and fixed incomes, a CCM program promotes preventative care and adherence to prescription regimens. This can lead to fewer hospitalizations, emergency room visits, and costly interventions.
- Drive New Clinic Revenue
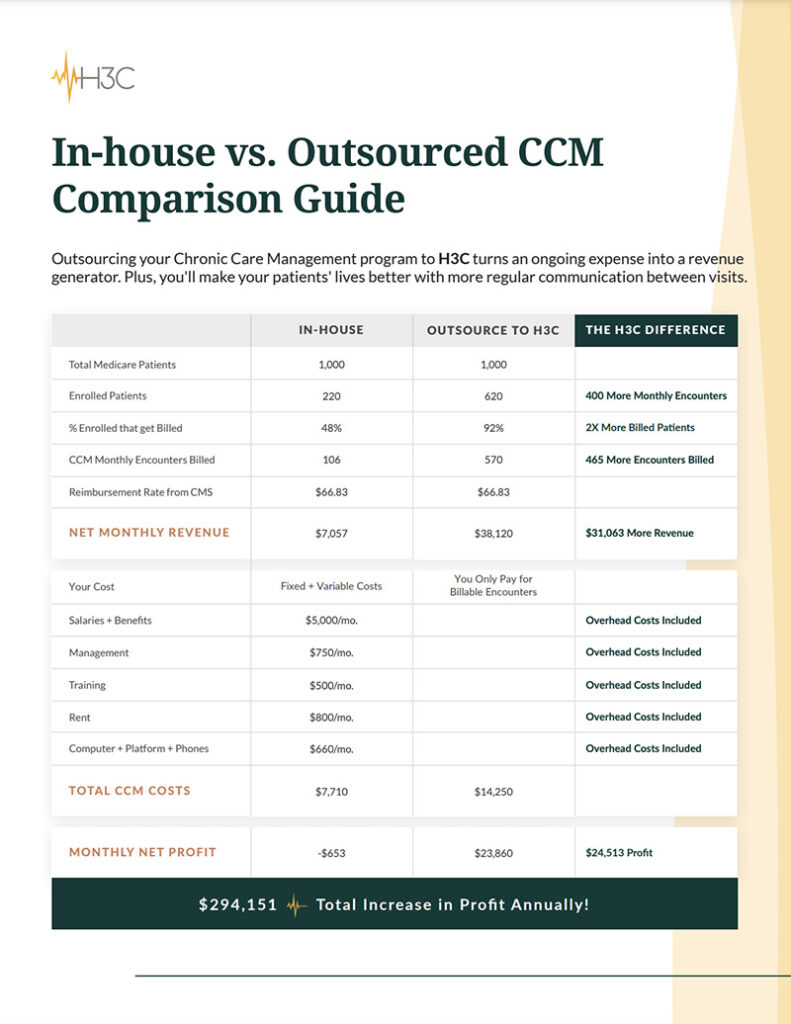
A well-established CCM program not only creates a more streamlined and informed approach to patient care, it can also increase revenue for your clinic. Through Medicare and Medicaid reimbursements, CCM services offer an additional revenue source for practices that provide care coordination for chronic disease management. This revenue can be reinvested in the clinic, allowing for the expansion of programs, staff, or services dedicated to improving outcomes for additional patient populations.
How Can H3C Support Continuity and Coordination of Patient Care?
Perhaps you’ve considered the advantages of implementing a CCM program at your clinic. But, the required time, staff and potential overhead costs don’t seem feasible. At H3C, we help clinics like yours outsource your CCM program quickly, easily and with no setup costs.
What to Expect From Your Successful, Outsourced CCM Program?
Once our dedicated enrollment specialists register your eligible patients, our staff of care coordinators and certified nurses facilitate monthly check-in calls. Your patients receive a dedicated H3C representative who understands their current medical challenges and can help them overcome barriers to care by:
- Connecting with the patient as a person, getting to know them and their challenges.
- Making appointments for the patient with the provider and any specialists who are needed for emerging issues.
- Providing medication check-ins and assistance with refills.
- Checking in on health plan and medication adherence, resolving any questions or problems.
- Collecting up-to-date information on the patient’s health and documenting those changes directly in your EMR. This ensures your staff has all the relevant patient information needed to provide great care in real time.
Your providers will have a more comprehensive view of their patient’s health, which maximizes time spent in office visits and improves overall patient satisfaction.