Proactive Engagement. Measurable Impact.
H3C reduces unnecessary utilization and helps avoid costly hospitalizations.

Proactive Engagement. Measurable Impact.
Health plans today are overwhelmed by rising costs tied to ER overuse and avoidable hospitalizations — especially in Medicaid populations.
Patients often wait until symptoms become emergencies. And by then, it’s too late.
Common challenges payers face:
Unnecessary ER visits driving millions in waste
Preventable hospitalizations going unflagged

Low patient compliance with treatment and medications
Quality penalties from missed screenings or poor engagement
Lack of real-time data to course-correct care plans
The H3C Solution: Engage Early. Act Smarter.
At H3C, we meet patients before they escalate into high-cost cases. Our team proactively addresses both clinical and non-clinical risk factors through tailored outreach and structured interventions.
Our programs utilize:
Social determinants of health (SDoH) screenings to surface social and behavioral barriers
Custom engagement protocols based on patient demographics, chronic conditions, and provider goals.
Escalation pathways to ensure early triage and avoid costly admissions.
Mental health and medication adherence assessments to address core risks.
Timely connections to PCPs, specialists, and community resources.
We prioritize the right level of care at the right time. Every patient is treated as a unique profile — no cookie-cutter scripts.
Why It Matters to You
With H3C, you’ll:
Lower avoidable utilization

Improve cost containment
Increase patient-level data to support payment justification
Enhance your plan’s reputation for health equity and proactive care
Learn how you can reduce unnecessary utilization and avoid costly hospitalizations
Generate extra revenue and add remote staff
at no added cost to you
There are no setup costs or out-of-pocket expenses for your clinic.
We’ll handle everything, from setup and enrollment to assessments and reporting and beyond.

Generate an average of $200,000+ per year net revenue (for clinics of 1,000 patients or more).
How much revenue could you generate for your organization?
- Federally Qualified Health Center (FQHC) or Rural Health Clinic (RHC)
- Primary Care Practice, Health System, or Other Type of Provider
Learn how to get started risk-free
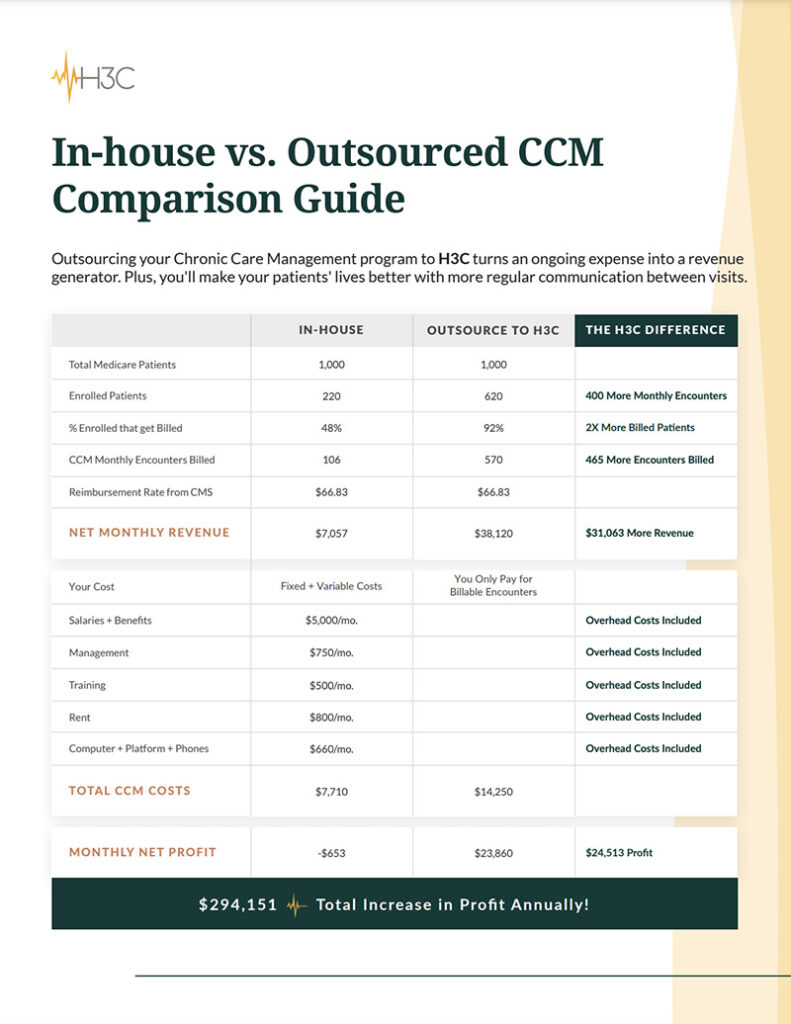
In-House vs. Outsourced CCM Comparison Guide
Outsourcing your Chronic Care Management program to H3C turns an ongoing expense into a revenue generator. Plus, you’ll make your patients’ lives better with more regular communication between visits.
We’ll do the rest
• Confirm patient eligibility and build out cohorts
• Schedule and conduct orientation sessions with your staff
• Create marketing materials
• Build out clinical pathway and care templates
• Craft encounter note summary templates
• Confirm program update process
• Send out welcome letters to patients
• Conduct EMR assessment
• Coordinate patient introductions
• Obtain and document patient consent
• Ensure compliance standards are met
• Connect with patient caregivers
• Complete intake assessment
• Conduct monthly patient calls, assessments, and pathways
• Review and update patient goals
• Carry out intervention plans
• Coordinate in-person patient appointments
• Provide referral assistance as needed
• Generate and upload care plans to EMR
• Mail care plans to patient
• Upload post-encounter summary notes
• Submit monthly risk level report
• Generate productivity reports
• Compile monthly billing reports


Primary Care Physician and Managing Partner
Complete patient care in 3 simple steps
You provide
the patients
Provide us with your patient list and we’ll handle the rest.
We contact
and enroll
We contact all eligible patients and work to enroll them in the
CCM program.
Complete care experience
We’ll conduct regular encounters and report back, providing patients the support they need to
stay healthy.
“I love that this program is available and I’m grateful that someone calls to check in on me.”
Deborah, 69

