Independent Practices find remote care management models are easier said than done
By Lindsay Arent RN, BSN, Director of Clinical Development, H3C
The COVID-19 pandemic drove most independent physician offices and rural health providers to increase acceptance and reliance on remote patient care models. While many saw the adoption of telehealth, chronic care management, and remote patient monitoring as inevitable, their accelerated use exposed some challenges, and at a time when independent practices were forced to think about their own survival, as well as caring for at-risk patient populations.
A recent survey conducted by The IPA Association of America (TIPAAA) found that 100% of respondents had realized a reduction in in-office patient visits, 83% had suffered a reduction in patient revenue, 67% had reduced office hours, and virtually all of them had increased their reliance on remote patient care.
It is a foregone conclusion that technology and, more specifically, remote patient care will continue to play a much more significant role in the future, with or without COVID-19. The question becomes:
How can the Independent Practice make the best use of the available options to optimize patient care while still continuing to remain profitable?
Independent physicians have attempted to address this question through use of Chronic Care Management (CCM). This five-year-old program offers an incentive to providers who conduct 20 minutes of remote care (phone or telehealth) for eligible Medicare patients who have two or more chronic conditions.
Up until the recent pandemic, CCM was widely publicized but scarcely utilized. COVID-19 has since changed all of that. All respondents to the TIPAAA survey are either participating or planning to launch Chronic Care Management programs. Both options of implementing a CCM program (do-it-yourself or outsourcing CCM to a third party) have their unique set of challenges.
H3C, a veteran of the Chronic Care Management space, has been the beneficiary of unsuccessful do-it-yourself programs, as well as the one to “clean up” failed attempts at outsourcing CCM programs.
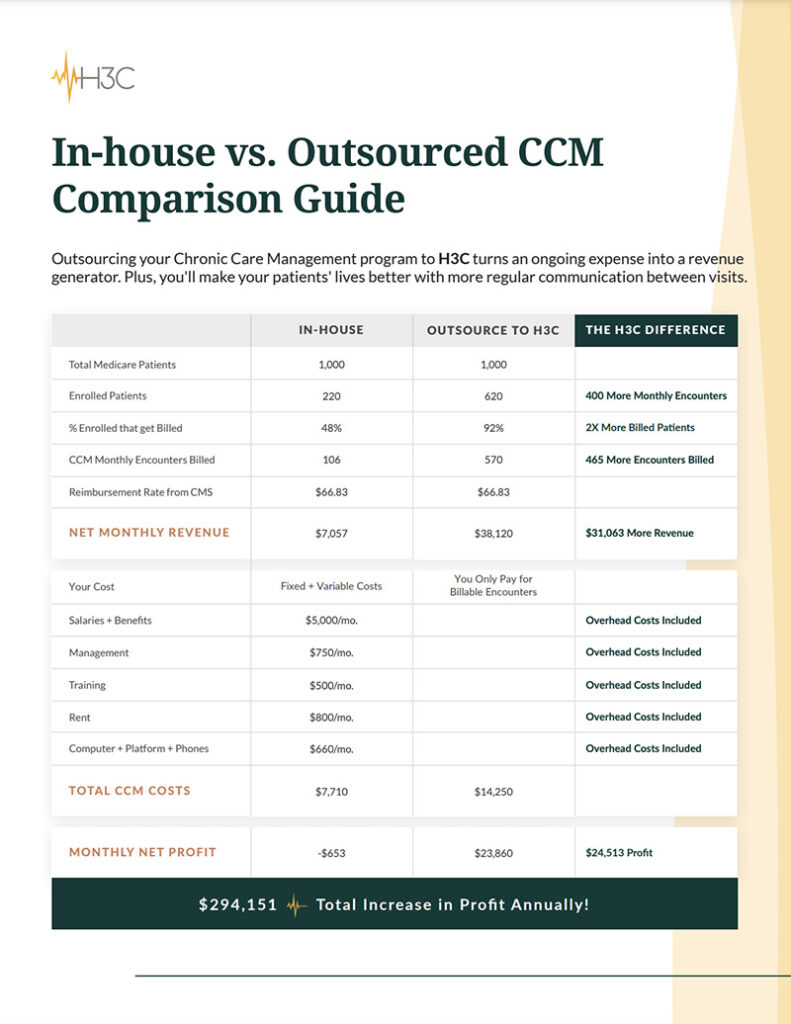
“It’s rare that a practice can effectively realize optimal clinical and financial results on their own, unless they are pretty small,” said Eric Wilson, CEO of H3C, an Omaha-based clinical call center company.
“Physician’s practices are built to provide care from patient-to-patient and are often in a ‘reactive’ mode to patient needs. As a result, putting a group of patients on a periodic call schedule always takes a back seat to seeing them face-to-face,” Wilson said. “Practices that want to do this on their own are quickly overwhelmed with the investment in technology, staffing, and the focus required to reach all eligible patients each month. The juice just isn’t worth the squeeze, unless they’re committed to re-designing the care model across their entire practice.”
“A physician’s office with, say, 1000 Medicare Patients, should expect that 75% of these patients would be eligible for a CCM program. Of those eligible, 70% should be enrolled and the practice should realize between $700,000 and $1,000,000 in incremental gross revenue for an effective CCM program. In our experience, most physician’s offices struggle to reach 25% of these levels when doing it themselves,” Wilson continued.
Practices that attempt a CCM program on their own typically have one or more of the following problems:
- They lack the technology and analytics platform to determine patient eligibility and efficiently manage CCM encounters over the phone.
- They lack the call center capability and mindset to ensure that every patient is prioritized and engaged every month.
- Their existing clinical staff is oriented to care for patients face-to-face and not remotely via telehealth. Typically, the patient experience suffers since clinical staff calling patients from their homes or cell phones lack experience or a strong platform to support them.
- As a result, providers realize far less than optimal financial results. A typical practice may only engage a fraction of its overall patient population each month. Clinicians are geared to provide care and not financial performance. Do-it-yourself CCM programs become a distraction and fail to provide an acceptable return on investment.
Similarly, outsourcing Chronic Care Management to a third-party provider is not a certain formula for success either. While there are many available options to outsource this activity, many of them come with their own set of problems. Common reasons that outsourced CCM programs fail to deliver include:
- Patients are not contacted each month and sometimes they are not even contacted at all.
- Once patients are enrolled, they often become “fatigued” by the same questions and answers each month, and program attrition rates are high.
- Outside vendors often put heavy demands on the need to integrate with existing EMR systems. As a result, implementation and “set up” requirements put stress on precious IT resources for a practice.
- In some cases, new platforms require heavy staff training during a time when clinical staffs are already taxed.
- Business models are just that – built for the vendor to benefit, without enough consideration given to the patient’s experience.
“We strive to speak to every patient every month and add value to every patient interaction. That’s the key to patient retention, in our view,” Wilson said. “To do this, we need a dynamic care platform that ensures we’re not asking them the same questions 12 times a year, and are tailoring our conversations to those unique needs of each patient. Sometimes that means we’re talking to them about their daughter’s graduation and not asking them if they’ve quit smoking 12 times a year. By setting the standard for patient contact high, we realize retention rates in excess of 90% over the course of a year. This stacks up very favorably versus all alternatives.”
Most providers would agree with the adage “what’s good for the patient, is good for my practice.” In today’s environment, that means the medical community needs to sometimes extend the definition of a practice beyond four walls, and also extend the eco-system of caregivers beyond those within a practice to effectively optimize the patient experience. Realizing favorable financial results is simply a by-product of the patient experience.