Table of Contents
One thing is for sure—healthcare is changing. Granted, that hasn’t stopped you from continuing to provide high-quality medicine to your patients.
But what if we told you that the top-notch care you’re currently providing could be enhanced?
What if you could connect with your vulnerable, high-risk patients monthly?
What if it were possible to not only speak with them, but take the time to provide them with valuable insights and education about their chronic conditions?
You’d likely earn yourself their loyalty for life. After all, why would they want to go anywhere else when they feel heard and looked after by you and your staff?
Sure, you’ve thought about this. But you have no idea how you would ever pull it off. Implementing a program like that will undoubtedly take more time, staff, and money than you have to spare right now.
And while you’re familiar with CCM programs, it seems like a lot of work and worry to get one fully implemented.
So, today we’re going down the list of the top four myths that are circling around CCM programs. Because integrating one into your clinic may not be as impossible as it seems.
Myth #1: Partnering with an external CCM organization puts my patients’ data at risk.
Keeping patient data protected is a high priority. Not only is it how you do business, it also happens to be the law. So, providing someone outside your organization with your patient list doesn’t feel quite right.
Will they take your patients?
Sell patient information?
No and no. A chronic care management program is exactly that—a program based in the world of medicine. As such, those providing these programs have the same feelings around patient privacy as you do—and will protect that privacy at all costs, the same as you or any other healthcare facility would.
Myth #2: My patients won’t be interested in a CCM program.
You think your patients won’t want to be bothered by a CCM program. After all, they have access to your clinic whenever they need you.
But therein lies the problem.
Patients scheduling themselves because an issue arises is a reactive approach. Most providers and clinics follow this approach. But it removes your patient’s ability to take control of their own health education.
But consider that the WHO believes 80% of chronic diseases could be eliminated by preventative measures. And in fact, two-thirds of all deaths in America are attributable to one of five chronic disorders: cancer, chronic obstructive pulmonary disease, diabetes, heart disease, and stroke.
Think about a patient you have who already has COPD and diabetes, and is now at risk for heart disease. They’re in annually for their physical and want to steer clear of getting heart disease. But year after year, their health inches closer to what they claim to want to avoid. Eventually it gets to a point where you feel your patient isn’t listening to your medical advice. You wish you could follow up with them on a regular basis to make sure they are following your treatment plan, but you simply don’t have time, and this patient gets lost in the shuffle amongst other annual patients. So, in all likelihood, they either succumb to heart disease or they leave your clinic for another that provides him/her with more communication in between their yearly visits to check on their progress (or lack of). Either way—a lose-lose, wouldn’t you agree?
But there’s another way. Enrolled in a CCM program, this patient would receive a call once per month to discuss their current health and the issue of heart disease. They could be monitored to ensure they are taking their medications and adhering to your treatment plans, and they could be educated on the importance of avoiding heart disease. A recent study suggests that health education for patients for follow-up of chronic diseases will significantly improve compliance to doctor’s advice regarding smoking, diet and exercise.
From daily and weekly habits your patient can change to reach better health to reminders about getting screened, a CCM program gives your patient more control over their own health because they feel educated and cared for.
Many patients actually find value in a CCM program, claiming they:
- Feel closer and better connected to their physician and healthcare team
- Want to take an active role in managing their overall health
- Feel a sense of comfort being spoken to every month
Through a CCM program, your high-risk patients are encouraged to take an active role in maintaining their health and compliance with their health plans. And as it’s completely optional to participate, patients will never feel pressured into joining.
Myth #3: A CCM program will further burden my already overburdened staff.
So, a CCM program is sounding better. But there’s still the matter of how taxing it will be on your existing staff. Your resources are already stretched thin and adding another patient program sounds downright impossible.
But with the right resources in place, a CCM program is there to make things easier so it doesn’t interrupt the day-to-day processes of nurses, physicians, and clinic staff. Rather it acts as an enhancer to your case management program. And should you decide to outsource your program with a CCM vendor, a good one will handle all the details from patient eligibility and enrollment to claims management and billing, and everything in between—all while working directly in your EMR system.
Ideally, the right partner will ask you to assign a primary “champion” or point of contact within your organization for twice-monthly updates. Your staff would see documentation, in real time, of every phone encounter their staff has with your patient. As a provider, you would also have access to risk stratification reports, giving you a broadened view of patient information.
It should also be noted that a patient need never know you’re outsourcing this service. The right partner will work as an extension of your office, down to the caller ID with your local exchange and clinic name. Care coordinators should represent themselves as a member of your clinic’s team.
And, perhaps most importantly, a CCM program in no way replaces the valuable people you already have in place at your office. Rather, it serves to make their lives easier, extending their delivery of quality care and ensuring your patients feel heard and well cared for so that you can retain them.
Myth #4: It’s difficult to bill for a CCM program.
In addition to being great for both your patients and your staff, a CCM program ultimately benefits your bottom line, too—and is incredibly easy to bill as there is just one billing code for this service: G0511.
Here’s how it works. CCM services are eligible for reimbursements through Medicare when they meet specific criteria around length of visit, care plan development, and ongoing outreach.
The code G0511 offers a reimbursement of $76.94 per encounter (per month). Here’s how that can break down for your practice:
1 patient = $76.94
500 patients x 1 call per month = $38,470
$38,470 x 12 months
$461,640 in incremental reimbursements
When you consider all the growth made possible for your clinic through that added revenue stream—more staff, new programs, updated resources—the bottom-line benefits become hard to ignore.
It doesn’t take long for a CCM program to be implemented into your practice, either. For most organizations, if done properly, full implementation could take a mere four to six weeks.
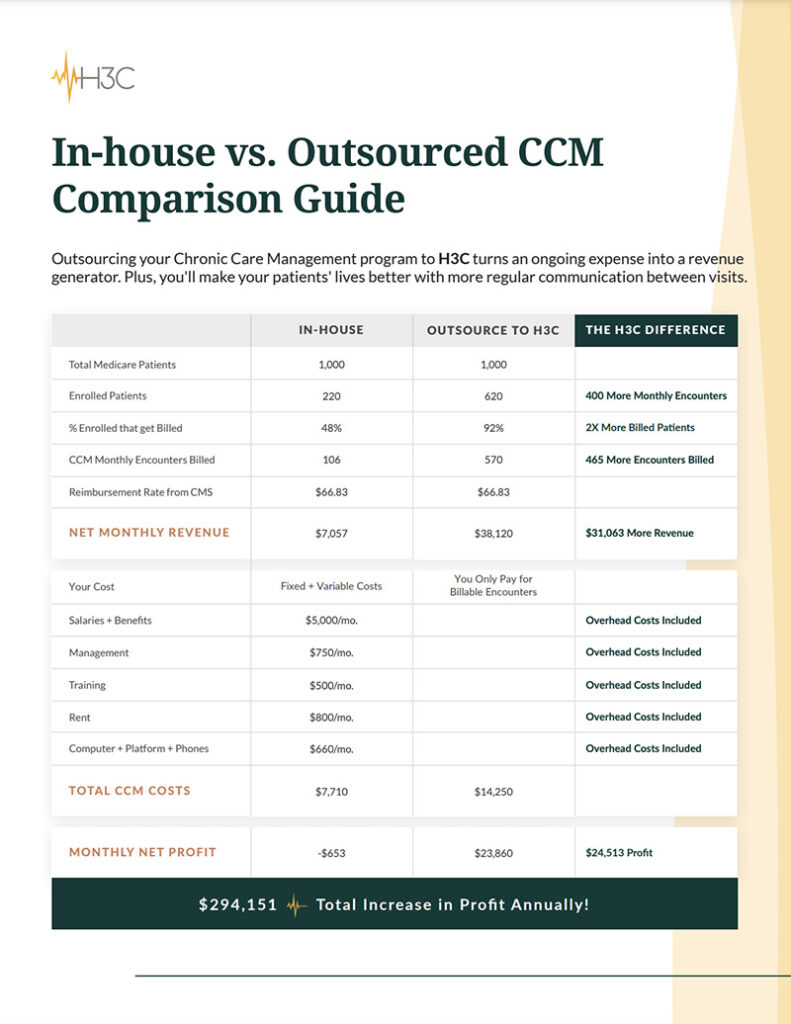
At H3C, not only do we provide our CCM program and technology at no cost to clinics, but we also help generate additional revenue to improve clinics and the care they provide. In fact, clinics that work with us soon discover that we’re one of their top sources of revenue. And as you can see, implementing a CCM program won’t prove difficult at all when you use the right partner.
According to CMS: Chronic care management is care coordination services done outside of the regular office visit for patients with multiple (two or more) chronic conditions expected to last at least 12 months or longer, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. These services are typically non-face-to-face and allow eligible practitioners to bill for at least 20 minutes or more of care coordination services per month.
A chronic care management program is exactly that—a program based in the world of medicine. As such, those providing these programs have the same feelings around patient privacy as you do—and will protect that privacy at all costs, the same as you or any other healthcare facility would.
H3C is an innovative healthcare solutions company combining exceptional patient-centric care with cutting-edge technology. Working as an extension of your clinic, we provide chronic care management that helps improve patient experiences and outcomes while boosting both clinical value and revenue. Schedule a call and let’s discuss how we can help you.